Medical Dermatology

General Skin Checks and Self-Monitoring
Dermatologists are regarded as the experts in the detection and treatment of all skin disorders including pre-cancerous skin lesions and skin cancers. As many early skin cancers are subtle and/or asymptomatic they may be missed by the untrained eye. The Dermatologists consulting at Inner Sydney Dermatology aim to ensure the early detection of pre-cancers and skin cancers, and offer patients the most suitable treatment options. They are also happy to instruct you on how to perform your own regular 'self skin examination' at home. The general recommendation from the Australasian College of Dermatologists is that patients should check their skin themselves every three months (the beginning of each season is an easy way to remember). If you are concerned about any skin lesions, make sure you arrange a consultation with your GP or Dermatologist. For those at high risk, or with a past history of skin cancer, we recommend a routine yearly skin check with your doctor.
Self-Monitoring
It is important to check your skin regularly to pick up any changes.
Look for:
- any crusty, non-healing sores/ulcers
- small lumps that are red, pale or pearly in colour
- new spots, freckles or any moles changing in colour, thickness or shape over a period of weeks to months (especially those dark brown to black, red or blue-black in colour).
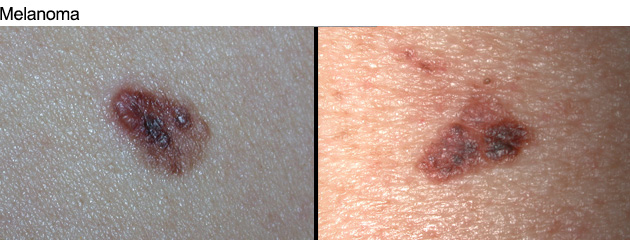
When checking your moles, look for the ABCDE of melanoma:
- Asymmetry
- Irregular Border
- Uneven Colour
- Diameter (usually over 6 mm)
- Evolving (ie. changing and growing).
Pre-Cancerous Sun Spots (Solar Keratoses)

Sun spots or Solar keratoses are pre-cancerous lesions usually found on sun-exposed skin. They most commonly appear as single, scattered or clustered rough, scaly patches. Sun spots are warning signs: they indicate that your skin has been damaged by ultraviolet (UV) radiation from sun exposure, and that you may be at risk of developing skin cancers.
These spots can sometimes disappear with strict sun avoidance and regular sunscreen use, but most persist and can become uncomfortable and unsightly. Solar keratoses of the lower lip is known as Actinic Cheilitis.
A proportion of sun spots can develop into an invasive form of skin cancer called Squamous Cell Carcinoma (SCC). Progression to SCC may be indicated by growth, discomfort/tenderness, persistent ulceration or bleeding.
The appearance of sun spots can vary, even on the same person. Early sun spots can often be more easily felt than seen, as rough sandpaper-like patches on the skin. They can also be sensitive, with a burning or stinging feeling especially in hot weather. Sun spots may appear as:
- a flat or slightly raised, scaly, skin coloured, red or brown patch
- a thickened or warty area
- a small horny outgrowth
People with fair skin over 40, and those who spend a lot of time outdoors are most at risk of developing sun spots.
Treatment of sun spots
The type of treatment recommended by your doctor will depend on the location, nature and number of sun spots you have. The most common types of treatments are listed below:Cryotherapy: Liquid nitrogen is used to freeze and destroy the damaged skin cells. This is usually used for small numbers of sun spots. The procedure stings, and the treated area forms a welt or blister, which crusts and usually heals over a couple of weeks. There is a small risk of leaving (permanent) white scars.
Curettage and Cautery: This is performed after the injection of local anaesthetic, and involves scraping away the abnormal tissue and sealing the wound using an electric current. This may be used for thicker sun spots or when early skin cancer is suspected. The treated area looks a little like a graze, takes a few weeks to heal (longer on the legs), and can leave an obvious scar.
‘Field Treatments’: If you have lots of sun spots it may not be practical to treat each spot individually, so a range of treatments are used that are applied to the whole affected area. These types of treatments have the advantage of treating not only visible sun spots, but also early microscopic ones which are not yet visible to the naked eye.
- Topical chemotherapy. This utilises a chemotherapy drug used to treat a number of different cancers. When used as a cream, it is absorbed by pre-cancerous skin cells and leads to their destruction. The cream is usually applied twice a day for about 2–4 weeks. The treated areas slowly become red, swollen, crusted and uncomfortable before settling down after treatment is stopped. Some people can develop more prolonged redness after use. As the cream can make you more sun sensitive, treatment is often recommended in the cooler months of the year.
- Topical immunotherapy. This works by stimulating the skin’s own immune system to attack and selectively destroy sun-damaged cells as well as reducing the occurrence of new sun spots. A cream is applied to affected skin according to your doctor’s instructions, usually 3 times a week for a period of 4 weeks. Your doctor then assesses the results and decides if another cycle of treatment is necessary. The reaction to this treatment varies from person to person, and most people experience some degree of inflammation of the skin with redness, scaling and crusting.
- Anti-inflammatory gel. This is a non-steroidal anti-inflammatory drug (NSAID) that interferes with the development of sun spots. The gel is usually applied to the skin twice daily for 3 months. Most people develop few side effects, apart from some scaling and flaking. While this form of therapy has the advantage of minimal ‘down time’, the long treatment period can be a problem, and longer term cure rates are not yet known.
- Photodynamic therapy (PDT). A cream containing a light-sensitising chemical is applied to the affected area and accumulates in sun damaged cells. These cells are then destroyed when the chemical is ‘activated’ after exposing the skin to a bright light source several hours later. The treatment can be quite painful. The treated area develops an uncomfortable ‘burn’: the area reddens, can blister, peel and become crusted while healing over about 2 weeks. Daylight PDT is a variation of this which utilises natural daylight rather than a light source to activate the chemical, and is particularly useful for treating facial sun spots.
- Laser and chemical peels can occasionally be used. There have been some recent studies using the Fraxel™ re:store laser for treatment of sun spots. Laser treatment is generally the treatment of choice for actinic cheilitis of the lower lip.
How can I help prevent sun spots developing?
Slip, slop and slap! Regular use of sun protection has been shown to help prevent and slow the development of sun spots.
Skin Cancers
The Dermatologists consulting at Inner Sydney Dermatology specialise in the management of pre-cancerous sunspots as well as skin cancers such as basal cell cancer, squamous cell cancer and melanoma.They can offer you an extensive range of treatments varying from conventional surgical therapies to newer topical treatment modalities where appropriate.
The best option will vary from person to person and will be individually tailored depending on the size, site and type of skin cancer.
Skin Cancer
Skin cancer occurs when the genetic material of skin cells is damaged, allowing them to grow in an uncontrolled way. One of the most important factors in causing this damage is prolonged exposure to ultraviolet (UV) radiation in the sun's rays, and it is thought that 95 to 99% of skin cancers in Australia are due to this. Over 200,000 Australians are treated for skin cancer each year and more than 1,000 Australians die from it every year.Skin cancers can be broadly divided into non-melanoma skin cancers (NMSC) and malignant melanoma (MM). The commonest forms of NMSC are basal cell carcinoma (BCC) and squamous cell carcinoma (SCC).
Fair-skinned Australians are at highest risk of developing both NMSC and MM, with exposure to sunlight in childhood and adolescence being a major risk factor. The risk of MM increases greatly with repeated episodes of sunburn, particularly if they occur before adulthood. Also at risk are people who have fair skin, increased numbers of unusual moles (dysplastic naevi), depressed immune systems, and a family or past history of MM. However, persistent moderate sun exposure over time increases the risks of both NMSC and MM.
Types of Skin Cancer
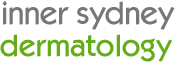
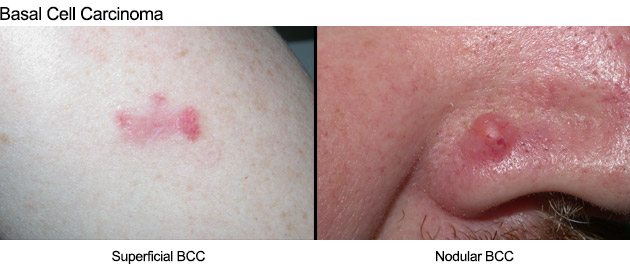
There are three main types of skin cancer:1. Basal Cell Carcinoma (BCC):
BCCs are the most common and least worrying type of skin cancer. They arise from cells in the lower part (basal layer) of the upper layer of the skin (epidermis) and tend to grow slowly. BCCs are most common on the face, head, neck and trunk regions. Nodular BCCs usually appear as a non-healing pimple-like lump, which may intermittently bleed, form an ulcer or scab. Superficial BCCs can appear as a red, scaly patch. The less common morphoeic or infiltrating BCCs can be subtle, appearing as a scar-like or shiny plaque on the skin. BCCs are locally destructive but are generally easily treated in their early stages. If left untreated they can grow and destroy adjoining structures, although they rarely spread throughout the body (metastasize).
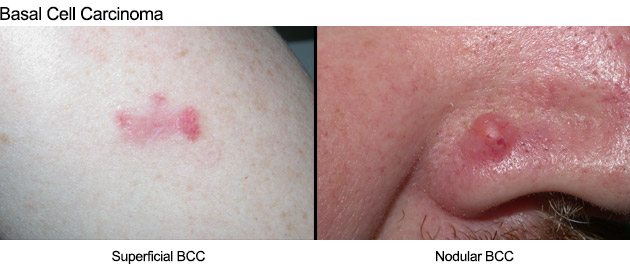
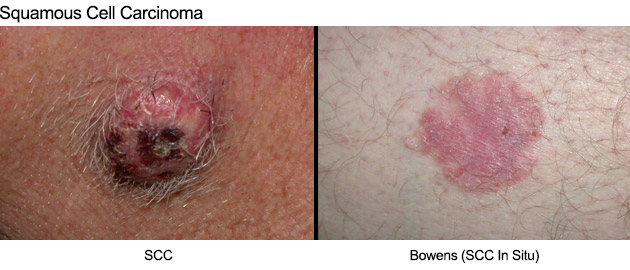
2. Squamous Cell Carcinoma (SCC)
SCCs are the second most common form of skin cancer. They tend to grow much faster than BCCs and most commonly occur on sun-exposed areas such as the face, ears, scalp, lips and backs of the hands. They can occasionally metastasize.
SCCs often appear as a fast-growing pink lump, or wart-like growth, which may have a central crater. They may also break down, crust, bleed and ulcerate. Occasionally they may be tender, or cause a burning or stinging sensation.
People who have had organ transplants, or are immunosuppressed for other reasons, are at higher risk of developing SCCs. Regular skin checks are particularly important in these groups because if an SCC does occur it can behave more aggressively, making treatment more difficult.
Bowen's Disease (SCC in situ) is an SCC which has not spread beyond the epidermis (the first layer of skin). They have no risk of spreading to other sites but can develop into an invasive SCC if left untreated. They are usually red, scaly patches and are quite common on lower legs and feet.
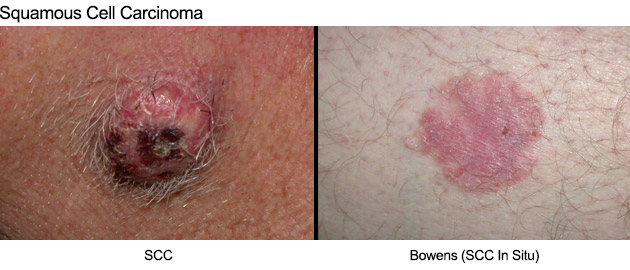
3. Malignant Melanoma (MM)
MMs are less common than BCCs and SCCs, but are much more dangerous. Australia has the world's highest incidence of melanoma and more than 1200 people die from melanoma each year. Like SCCs and BCCs, melanomas can occur on sun-exposed skin, but they also occur on skin that is usually covered, but has been sunburnt in the past. Malignant melanomas may metastasize and cause death.
Most MM start as a new, often dark spot that continues to change. They may also occur in moles which may have been present for years but then change their appearance. Most melanomas are usually asymptomatic, though uncommonly present with itch, or bleeding in the absence of trauma.
See also the ABCDE of melanoma (see Self-Monitoring).
Skin Cancer Treatment

Several types of skin cancer treatment are now available, ranging from surgical options to creams and light treatments. Your Dermatologist will advise you on the different types of treatments that may be suitable for you depending on the type, site, size and depth of your skin cancer.
Dermatologic Surgery
Most invasive skin cancers are treated with surgery where possible. Surgery has the benefits of a high cure, minimal downtime, and generally good cosmetic results. Apart from using the best surgical techniques, Dermatologists can also advise you on how to minimise any scarring.
Mohs’ Surgery
Mohs’ Surgery is the ‘gold standard’ of treatment for difficult and recurrent skin cancers, or those in cosmetically important sites such as the nose or upper lip. It has the highest cure rate of any treatment modality.
Topical Immunotherapy
This involves the application of a cream which stimulates the skin’s own immune system to attack and selectively destroy the skin cancer cells. It is only appropriate for certain superficial and low-grade skin cancers, and is usually applied 5 nights a week for a period of 6 weeks. The reaction to this treatment varies from person to person, and most people experience inflammation of the skin with redness, scaling and crusting.
Curettage and Cautery
This techniques involves 'scraping and burning' the skin cancer cells away. The area is numbed using a local anaesthetic and then the lesion is scraped away and a gentle electric current applied to the base to seal the blood vessels and destroy any residual skin cancer cells. No sutures are required and the lesion heals slowly, much like a deep graze would. It is only suitable for certain, usually superficial skin cancers in particular sites, and can leave obvious scars.
Topical chemotherapy
This utilises a chemotherapy drug used to treat a number of different cancers. When used as a cream, it is absorbed by cancerous skin cells and leads to their destruction. It is only appropriate for certain superficial and low-grade skin cancers, and is usually applied twice a day for about 3–6 weeks. The treated areas usually become red, swollen, crusted and uncomfortable before settling down after treatment is stopped.Photodynamic therapy (PDT). A cream containing a light-sensitising chemical is applied to the affected area and accumulates in cancerous cells. These cells are then destroyed when the chemical is ‘activated’ after exposing the skin to a bright light source several hours later. The treatment can be quite painful and the area develops an uncomfortable ‘burn’: the area reddens, can blister, peel and become crusted while healing over about 2 weeks. 2 treatments are generally required. It is only suitable for some superficial skin cancers and cure rates are much lower than other modalities. There have been some concerning reports of more aggressive skin cancers developing in treated areas.
Excessive Sweating (Hyperhidrosis)
Excessive underarm sweating (or hyperhidrosis) can be treated using the same injections that are used to relax facial muscles and target wrinkles. After the application of anaesthetic cream a series of small injections are performed to the armpit area. The active protein enters the sweat glands and blocks the release of chemicals that signal perspiration. After treatment, it normally takes 1-3 weeks to see the full effect, which lasts for 6-9 months in most people. This is a simple procedure that can be done in the Dermatologist’s office and usually takes around 15 minutes.A Medicare rebate may be available for patients who have failed treatment with Driclor deodorant if treated by a Medicare-approved specialist. Dr Andrew Ming is approved to treat patients with severe underarm sweating under this scheme. This dramatically reduces out-of-pocket costs for patients, who can have up to 3 treatments a year.
Acne and Acne Scarring
 The Dermatologists consulting at Inner Sydney Dermatology specialise in the treatment of acne and acne scarring.
The Dermatologists consulting at Inner Sydney Dermatology specialise in the treatment of acne and acne scarring.Acne is a common disorder of the oil or sebaceous glands, which causes pimples. It occurs when the openings to the oil glands (pores) become blocked, allowing a build up of oil and bacteria, and subsequent inflammation. The clinical features vary from person to person and can include blackheads, whiteheads, pustules and/or nodules or cysts. Acne generally occurs in areas where there is a high concentration of oil glands ie. the face, chest, upper back, shoulders, neck. Although acne is most commonly seen in teenagers, it can affect people of all ages.
Acne can be triggered by hormonal changes during puberty, pregnancy or the menstrual cycle. However, acne an also be aggravated by stress, some medications, make-ups or face creams, and other external or environmental factors. Genetics also plays a role, as acne often runs in families. The role of diet has always been controversial but some studies have shown a reduction in acne in patients consuming a low GI (glycaemic index) diet.
Treatment
Acne treatment needs to be individualised, based on the type of acne and severity, and the patient’s general health and preferences. Early treatment is encouraged to prevent or minimise scarring.
Anti acne cleansers
These contain active ingredients which help unblock pores, and/or reduce oil production and inflammation (eg. salicylic acid, alpha hydroxy acids, nicotinamide)
Topical treatments
These generally work by killing or slowing the growth of bacteria, reducing oil production and inflammation, unblocking pores or combinations of the above. They include:
- Benzoyl peroxide
- Topical antibiotics
- Vitamin A analogue creams
- Azelaic acid
Oral medications
- Oral antibiotics. These are used for their anti-bacterial and anti-inflammatory effects. It generally takes up to 2 months to see a result and most patients need to stay on these medications for at least 6 months.
- Hormonal treatment. In some women certain oral contraceptive pills and other anti-androgen hormones can be useful in controlling acne.
- Oral retinoids (vitamin A analogues)
. These are generally reserved for patients with severe acne, or those who have failed other oral therapies. They work by shrinking the oil glands, thus reducing the production of oil and pore blockage, and the development of new acne lesions. They can only be prescribed by Dermatologists and some specialist GPs, and require regular monitoring.
Acne scarring
Acne scarring can cause significant psychological stress for those affected, and effective treatment is a specialised area of Dermatology. As there are many different types of acne scarring, treatment needs to be individualized. Acne scarring can appear as flat marks (which can be red, white or brown), raised or thickened areas, or indented or pitted areas of skin.
Treatment
Treatment of acne scarring usually involves repeated treatments over a number of months to achieve the best results, and often a combination of therapies are required. Although it is generally not possible to completely eliminate scarring, significant improvement can be achieved using several specialized techniques.Your Dermatologist will recommend a treatment plan that is tailored to your particular skin type and scarring.
Treatments include:
Cortisone injections
These are used for thickened or keloid scars to help flatten them. Usually a series of injections are required, approximately 6 weeks apart.
Subcision
Subcision is a simple procedure that can be used to improve deeply indented acne scars which are 'pulled down' by bands of fibrous scar tissue. The affected area is numbed using local anaesthetic, and a needle is inserted under the scar and swept backwards and forwards and side to side to break up these fibrous bands. Once the scar tissue is released, the skin is free to lift up to its normal position. This procedure usually results in some bruising and swelling, although the bruising also helps stimulate collagen production which has a filling effect. Multiple treatments are usually performed at two to three-monthly intervals until the desired result is achieved. This treatment is often combined with other treatments such as laser therapy.
Fractional Laser
Fractional non-ablative laser can be used to improve the appearance of acne scars by remodelling the skin and stimulating new collagen production (the main support structure of skin). These revolutionary devices use pinpoint laser beams to create thousands of microscopic holes in the skin. This stimulates the body's own natural healing process which stimulates the production of collagen in areas of loss, and replacement of old damaged collagen with new collagen, leading to smoothing and filling of acne scars. Unlike other laser treatments, fractional laser can be used on any area of the body and in all skin types. Typically a series of 3-5 laser treatments are recommended at regular intervals.
Fractional Radiofrequency
Micro-Needle Fractional Radiofrequency (FRF) utilises minimally invasive micro-needles to deliver controlled radiofrequency (RF) energy directly into various depths of the skin, stimulating collagen remodelling and improving acne scarring. It can be used on all skin types, with very low risk of side effects and reactive pigmentation – a very important feature when treating skin of colour. The RF energy is delivered through the focused tip of the micro-needles, minimising trauma to the surrounding skin surface. Fractional Radiofrequency is indicated for various skin conditions including hyperpigmentation, deep and shallow wrinkles, and acne scarring.
Punch excisions
This can be used to remove some small and deep acne scars. The procedure is performed under local anaesthetic, using a circular device called a punch biopsy, which works much like an apple corer to remove the scar. The edges of normal skin are then carefully sutured together. Punch excision is generally combined with laser treatment after healing to optimize cosmetic results.
Fillers
Fillers are natural gel products that can be used to improve indented or depressed acne scars. After the application of local anaesthetic cream, they are injected directly underneath scars to fill the hollowed area. Although fillers are not permanent, they generally last months to years, and over time stimulate the production of collagen (one of the support structures in skin) which helps hold the scar in its new position. Fillers can also be combined with other treatments such as subcision and laser.
Rosacea

Rosacea is a chronic condition that primarily affects the central face. It is characterized by
- a tendency to flush and blush
- facial redness
- broken capillaries
- episodes of inflammation (resulting in pimple-like spots)
- swelling, which can be intermittent or persistent
The disorder is more common in fair skinned, young-middle aged women and develops slowly over time, gradually worsening if not treated. In some people, especially men, thickening and lumpiness may develop on the nose, which may appear swollen (rhinophyma). The eyes may also be involved resulting in grittiness, redness and irritation.The cause of rosacea is unknown. Although various theories have implicated bacteria, mites, a fungus, a disturbance of connective tissue under the skin, or psychological factors, none have been proven. It seems likely that there is no single cause of rosacea and that it develops in individuals who are susceptible due to a variety of factors such as heredity, skin colour, skin structure, and immune response.
Factors that can aggravate rosacea include:
- hot liquids
- alcoholic beverages
- spicy foods
- sun exposure
- extremes of temperature
- exercise
- emotional influences
- certain medications
Although there is no cure for rosacea at present, various treatments can reduce or eliminate the symptoms of rosacea, and may slow or even stop its progression.
In general, patients should avoid factors that produce facial flushing or irritate the skin.
Treatment
Various treatments, both topical and oral, can be used to control redness and reduce the number of papules and pustules. A combination of treatments may sometimes be required.Generally, only gentle cleansers and moisturisers should be used on the face, in combination with a low irritant sunscreen. Agents containing alcohol or other irritating ingredients should be avoided.
Topical Agents: The most commonly used topical preparations are antibacterial agents, azelaiec acid or botanical extracts, which are generally applied twice daily to to a clean, dry face. Topical medications usually produce some improvement within three to four weeks, but may take up to two months to show maximum improvement.
Vasoconstricting agents: When applied to the skin, these cause surface blood vessels to constrict, resulting in a reduction in facial redness which generally lasts 12 hours.
Oral Agents: The tetracycline group of antibiotics is most commonly used. Oral medications are usually taken once or twice daily and tend to produce results more quickly than topical medications, but usually need to be taken for several weeks to months. Some patients require low-dose maintenance therapy.
Laser and Light: Vascular lasers (such as Vbeam® Perfecta Pulsed Dye Laser) and BroadBand Light (BBL) can be used to eliminate redness and broken capillaries, reduce pore size and improve skin texture. However, these changes can recur over time (generally years), particularly if flushing triggers are not avoided.
Resurfacing or Fractional lasers or surgery can also be used to correct the nose enlargement in people with rhinophyma.
Eczema
 Eczema is a common skin condition, which affects one in three Australians. The terms 'eczema' and 'dermatitis' are often used interchangeably, and refer to a group of recurring inflammatory skin conditions with similar changes. Eczema can vary in appearance but is usually characterized by areas of red, itchy, scaly skin, sometimes with weeping, oozing or crusting (especially if infected from scratching). Repeated scratching may cause the skin to become thickened and sometimes darkened in colour.
Eczema is a common skin condition, which affects one in three Australians. The terms 'eczema' and 'dermatitis' are often used interchangeably, and refer to a group of recurring inflammatory skin conditions with similar changes. Eczema can vary in appearance but is usually characterized by areas of red, itchy, scaly skin, sometimes with weeping, oozing or crusting (especially if infected from scratching). Repeated scratching may cause the skin to become thickened and sometimes darkened in colour.Different forms of eczema exist including atopic eczema, discoid eczema, eczema craquele, venous eczema and irritant or allergic contact dermatitis. They are usually distinguished based on the history, clinical appearance, age of onset and the areas affected. Atopic eczema often begins in childhood, and may improve or even disappear as children get older. It classically affects the face, neck and creases of the elbows and knees. In younger children though, the location of eczema can be quite different.
The exact cause of eczema is unknown, however genetic factors play a role as it often runs in families. Patients with eczema have a problem with their skin barrier function. Not only is water lost from the skin leaving it dry and scaly, but the skin is vulnerable to irritants, allergens and infections. The use of regular moisturizers is therefore crucial in the management of eczema.
In addition to problems with the skin barrier function, there is an imbalance of the skin’s immune system. Often there is a history of atopy i.e. eczema, asthma or hayfever, as well as other allergies in the patient or family members.
There are a number of recognized factors that can trigger or exacerbate eczema and these include house dust mite, moulds, pet fur, changes in weather or humidity, soaps and shampoos, other irritants (including cosmetics chemicals, perfumes, grasses, pollens, sand, harsh clothing such as wool), and sometimes certain foods or stress.

Treatment
Eczema is often a long-term problem. Although the tendency to eczema cannot be cured, the condition can be controlled. An important aspect of treatment is identifying and minimizing any aggravating factors, and maintaining the skin’s protective barrier function. The following steps and treatments can be used to manage eczema:
- Avoid Irritants: protect the skin from exposure to water and detergents, chemicals, dust etc
- Bathing: avoid long hot showers (use lukewarm water) or prolonged baths. Uses a soap-free wash instead of soap, or bath oil
- Clothing: wear soft, breathable fabrics. Avoid rough fabrics such as wool and some synthetics
- Moisturisers: apply perfume-free creams or ointments liberally and often, especially after showering or swimming
- Steroid creams and ointments: these may be prescribed by your Dermatologist and applied to the affected patches of skin to reduce inflammation and itching. Providing they are used as instructed they are perfectly safe, even for baby’s skin
- Other prescription anti-inflammatory creams: can sometimes be used instead of topical steroids
- Antibiotics: these may be prescribed by your Dermatologist if your eczema is infected (most commonly due to Staphylococcus Aureus)
- Anti-Histamines: these may be used to help reduce itching
- Wet dressings: wet bandages are often used in combination with moisturisers and steroid creams to help soothe the skin
- Other: more severe cases of eczema may require light treatment (phototherapy) or stronger oral medications
Psoriasis
 Psoriasis is a chronic inflammatory skin condition characterized by well-defined, red patches or plaques (thickened skin) often with a silvery scale, which may or may not be itchy.
Psoriasis is a chronic inflammatory skin condition characterized by well-defined, red patches or plaques (thickened skin) often with a silvery scale, which may or may not be itchy.Psoriasis can start at any age including childhood, but is most common in adulthood. It affects males and females equally and about one third of patients have a family history of the condition. Although genetic factors are important, the disease is thought to be an inflammatory disorder related to 'over-activation' of the immune system.
Psoriasis most commonly presents as symmetrical red, scaly patches and plaques on the elbows, knees, lower back and scalp, although any part of the skin can be involved including the palms and soles, skin creases and genital area. It can also affect the nails, and occasionally the joints (psoriatic arthritis).
There are several different types of psoriasis, which vary in their appearance. These include:
- Scalp psoriasis: often the first or only affected area
- Chronic plaque psoriasis: red patches and plaques of varying sizes appear and usually have a silvery white scale. This type can occur anywhere on the skin but commonly affects the elbows, knees, scalp and lower back
- Acute guttate psoriasis: widespread, small plaques appear on the trunk and limbs, often following a Strep throat infection
- Flexural or inverse psoriasis: shiny, red and sometimes fissured and painful patches affect the skin folds (armpits, groin creases, under the breasts, genitals and buttocks). Sometimes the areas become secondarily infected with Candida
- Pustular psoriasis: multiple small red pustules appear on the skin, often associated with other symptoms such as fevers and pain
- Palmoplantar psoriasis: affects the palms and or soles, and is often associated with thickening of the skin and painful fissures
- Nail psoriasis: pitting, ridging, discolouration and lifting of the nails can occur
Psoriasis can be aggravated by a number of factors including infection, skin injury, smoking, alcohol, obesity, stress, weather and certain medications.
Treatment
Although there is no cure for psoriasis, the condition can be managed to reduce its symptoms and appearance. Treatment needs to be individualized according to the type of psoriasis, and its extent and severity. This includes avoidance of exacerbating factors such as smoking and alcohol, often in combination with other therapies such as:
- Mositurisers: to reduce skin dryness and scaling
- Tar based or other medicated shampoos
- Creams, ointments or lotions prescribed by your Dermatologist: these may include tar based preparations, Vitamin D analogues, topical steroids and other anti-inflammatory creams
- Phototherapy (light therapy) such as Narrow Band UVB
- Oral medicines for more severe psoriasis
- Biologics: a relatively new type of treatment generally given my injection and reserved for patients with conventional treatment-resistant psoriasis
Paediatric Dermatology
 Children require special care in many areas, and their skin health is no exception. Children are more prone to certain dermatological conditions, which can be distressing if not managed properly. These include eczema (dermatitis), infections such as impetigo, viral rashes, warts and psoriasis. Dr Andrew Ming specializes in the treatment of all aspects of Paediatric Dermatology and offers a comprehensive range of services specifically for children and adolescents.
Children require special care in many areas, and their skin health is no exception. Children are more prone to certain dermatological conditions, which can be distressing if not managed properly. These include eczema (dermatitis), infections such as impetigo, viral rashes, warts and psoriasis. Dr Andrew Ming specializes in the treatment of all aspects of Paediatric Dermatology and offers a comprehensive range of services specifically for children and adolescents.
 Sun spots or Solar keratoses are pre-cancerous lesions usually found on sun-exposed skin. They most commonly appear as single, scattered or clustered rough, scaly patches. Sun spots are warning signs: they indicate that your skin has been damaged by ultraviolet (UV) radiation from sun exposure, and that you may be at risk of developing skin cancers.
These spots can sometimes disappear with strict sun avoidance and regular sunscreen use, but most persist and can become uncomfortable and unsightly. Solar keratoses of the lower lip is known as Actinic Cheilitis.
A proportion of sun spots can develop into an invasive form of skin cancer called Squamous Cell Carcinoma (SCC). Progression to SCC may be indicated by growth, discomfort/tenderness, persistent ulceration or bleeding.
The appearance of sun spots can vary, even on the same person. Early sun spots can often be more easily felt than seen, as rough sandpaper-like patches on the skin. They can also be sensitive, with a burning or stinging feeling especially in hot weather. Sun spots may appear as:
Sun spots or Solar keratoses are pre-cancerous lesions usually found on sun-exposed skin. They most commonly appear as single, scattered or clustered rough, scaly patches. Sun spots are warning signs: they indicate that your skin has been damaged by ultraviolet (UV) radiation from sun exposure, and that you may be at risk of developing skin cancers.
These spots can sometimes disappear with strict sun avoidance and regular sunscreen use, but most persist and can become uncomfortable and unsightly. Solar keratoses of the lower lip is known as Actinic Cheilitis.
A proportion of sun spots can develop into an invasive form of skin cancer called Squamous Cell Carcinoma (SCC). Progression to SCC may be indicated by growth, discomfort/tenderness, persistent ulceration or bleeding.
The appearance of sun spots can vary, even on the same person. Early sun spots can often be more easily felt than seen, as rough sandpaper-like patches on the skin. They can also be sensitive, with a burning or stinging feeling especially in hot weather. Sun spots may appear as:
 2. Squamous Cell Carcinoma (SCC)
SCCs are the second most common form of skin cancer. They tend to grow much faster than BCCs and most commonly occur on sun-exposed areas such as the face, ears, scalp, lips and backs of the hands. They can occasionally metastasize.
SCCs often appear as a fast-growing pink lump, or wart-like growth, which may have a central crater. They may also break down, crust, bleed and ulcerate. Occasionally they may be tender, or cause a burning or stinging sensation.
People who have had organ transplants, or are immunosuppressed for other reasons, are at higher risk of developing SCCs. Regular skin checks are particularly important in these groups because if an SCC does occur it can behave more aggressively, making treatment more difficult.
Bowen's Disease (SCC in situ) is an SCC which has not spread beyond the epidermis (the first layer of skin). They have no risk of spreading to other sites but can develop into an invasive SCC if left untreated. They are usually red, scaly patches and are quite common on lower legs and feet.
2. Squamous Cell Carcinoma (SCC)
SCCs are the second most common form of skin cancer. They tend to grow much faster than BCCs and most commonly occur on sun-exposed areas such as the face, ears, scalp, lips and backs of the hands. They can occasionally metastasize.
SCCs often appear as a fast-growing pink lump, or wart-like growth, which may have a central crater. They may also break down, crust, bleed and ulcerate. Occasionally they may be tender, or cause a burning or stinging sensation.
People who have had organ transplants, or are immunosuppressed for other reasons, are at higher risk of developing SCCs. Regular skin checks are particularly important in these groups because if an SCC does occur it can behave more aggressively, making treatment more difficult.
Bowen's Disease (SCC in situ) is an SCC which has not spread beyond the epidermis (the first layer of skin). They have no risk of spreading to other sites but can develop into an invasive SCC if left untreated. They are usually red, scaly patches and are quite common on lower legs and feet.
 3. Malignant Melanoma (MM)
MMs are less common than BCCs and SCCs, but are much more dangerous. Australia has the world's highest incidence of melanoma and more than 1200 people die from melanoma each year. Like SCCs and BCCs, melanomas can occur on sun-exposed skin, but they also occur on skin that is usually covered, but has been sunburnt in the past. Malignant melanomas may metastasize and cause death.
Most MM start as a new, often dark spot that continues to change. They may also occur in moles which may have been present for years but then change their appearance. Most melanomas are usually asymptomatic, though uncommonly present with itch, or bleeding in the absence of trauma.
3. Malignant Melanoma (MM)
MMs are less common than BCCs and SCCs, but are much more dangerous. Australia has the world's highest incidence of melanoma and more than 1200 people die from melanoma each year. Like SCCs and BCCs, melanomas can occur on sun-exposed skin, but they also occur on skin that is usually covered, but has been sunburnt in the past. Malignant melanomas may metastasize and cause death.
Most MM start as a new, often dark spot that continues to change. They may also occur in moles which may have been present for years but then change their appearance. Most melanomas are usually asymptomatic, though uncommonly present with itch, or bleeding in the absence of trauma.
 Several types of skin cancer treatment are now available, ranging from surgical options to creams and light treatments. Your Dermatologist will advise you on the different types of treatments that may be suitable for you depending on the type, site, size and depth of your skin cancer.
Several types of skin cancer treatment are now available, ranging from surgical options to creams and light treatments. Your Dermatologist will advise you on the different types of treatments that may be suitable for you depending on the type, site, size and depth of your skin cancer.
 The Dermatologists consulting at Inner Sydney Dermatology specialise in the treatment of acne and acne scarring.
Acne is a common disorder of the oil or sebaceous glands, which causes pimples. It occurs when the openings to the oil glands (pores) become blocked, allowing a build up of oil and bacteria, and subsequent inflammation. The clinical features vary from person to person and can include blackheads, whiteheads, pustules and/or nodules or cysts. Acne generally occurs in areas where there is a high concentration of oil glands ie. the face, chest, upper back, shoulders, neck. Although acne is most commonly seen in teenagers, it can affect people of all ages.
Acne can be triggered by hormonal changes during puberty, pregnancy or the menstrual cycle. However, acne an also be aggravated by stress, some medications, make-ups or face creams, and other external or environmental factors. Genetics also plays a role, as acne often runs in families. The role of diet has always been controversial but some studies have shown a reduction in acne in patients consuming a low GI (glycaemic index) diet.
The Dermatologists consulting at Inner Sydney Dermatology specialise in the treatment of acne and acne scarring.
Acne is a common disorder of the oil or sebaceous glands, which causes pimples. It occurs when the openings to the oil glands (pores) become blocked, allowing a build up of oil and bacteria, and subsequent inflammation. The clinical features vary from person to person and can include blackheads, whiteheads, pustules and/or nodules or cysts. Acne generally occurs in areas where there is a high concentration of oil glands ie. the face, chest, upper back, shoulders, neck. Although acne is most commonly seen in teenagers, it can affect people of all ages.
Acne can be triggered by hormonal changes during puberty, pregnancy or the menstrual cycle. However, acne an also be aggravated by stress, some medications, make-ups or face creams, and other external or environmental factors. Genetics also plays a role, as acne often runs in families. The role of diet has always been controversial but some studies have shown a reduction in acne in patients consuming a low GI (glycaemic index) diet.
 Rosacea is a chronic condition that primarily affects the central face. It is characterized by
Rosacea is a chronic condition that primarily affects the central face. It is characterized by
 Eczema is a common skin condition, which affects one in three Australians. The terms 'eczema' and 'dermatitis' are often used interchangeably, and refer to a group of recurring inflammatory skin conditions with similar changes. Eczema can vary in appearance but is usually characterized by areas of red, itchy, scaly skin, sometimes with weeping, oozing or crusting (especially if infected from scratching). Repeated scratching may cause the skin to become thickened and sometimes darkened in colour.
Different forms of eczema exist including atopic eczema, discoid eczema, eczema craquele, venous eczema and irritant or allergic contact dermatitis. They are usually distinguished based on the history, clinical appearance, age of onset and the areas affected. Atopic eczema often begins in childhood, and may improve or even disappear as children get older. It classically affects the face, neck and creases of the elbows and knees. In younger children though, the location of eczema can be quite different.
The exact cause of eczema is unknown, however genetic factors play a role as it often runs in families. Patients with eczema have a problem with their skin barrier function. Not only is water lost from the skin leaving it dry and scaly, but the skin is vulnerable to irritants, allergens and infections. The use of regular moisturizers is therefore crucial in the management of eczema.
In addition to problems with the skin barrier function, there is an imbalance of the skin’s immune system. Often there is a history of atopy i.e. eczema, asthma or hayfever, as well as other allergies in the patient or family members.
There are a number of recognized factors that can trigger or exacerbate eczema and these include house dust mite, moulds, pet fur, changes in weather or humidity, soaps and shampoos, other irritants (including cosmetics chemicals, perfumes, grasses, pollens, sand, harsh clothing such as wool), and sometimes certain foods or stress.
Eczema is a common skin condition, which affects one in three Australians. The terms 'eczema' and 'dermatitis' are often used interchangeably, and refer to a group of recurring inflammatory skin conditions with similar changes. Eczema can vary in appearance but is usually characterized by areas of red, itchy, scaly skin, sometimes with weeping, oozing or crusting (especially if infected from scratching). Repeated scratching may cause the skin to become thickened and sometimes darkened in colour.
Different forms of eczema exist including atopic eczema, discoid eczema, eczema craquele, venous eczema and irritant or allergic contact dermatitis. They are usually distinguished based on the history, clinical appearance, age of onset and the areas affected. Atopic eczema often begins in childhood, and may improve or even disappear as children get older. It classically affects the face, neck and creases of the elbows and knees. In younger children though, the location of eczema can be quite different.
The exact cause of eczema is unknown, however genetic factors play a role as it often runs in families. Patients with eczema have a problem with their skin barrier function. Not only is water lost from the skin leaving it dry and scaly, but the skin is vulnerable to irritants, allergens and infections. The use of regular moisturizers is therefore crucial in the management of eczema.
In addition to problems with the skin barrier function, there is an imbalance of the skin’s immune system. Often there is a history of atopy i.e. eczema, asthma or hayfever, as well as other allergies in the patient or family members.
There are a number of recognized factors that can trigger or exacerbate eczema and these include house dust mite, moulds, pet fur, changes in weather or humidity, soaps and shampoos, other irritants (including cosmetics chemicals, perfumes, grasses, pollens, sand, harsh clothing such as wool), and sometimes certain foods or stress.

 Psoriasis is a chronic inflammatory skin condition characterized by well-defined, red patches or plaques (thickened skin) often with a silvery scale, which may or may not be itchy.
Psoriasis can start at any age including childhood, but is most common in adulthood. It affects males and females equally and about one third of patients have a family history of the condition. Although genetic factors are important, the disease is thought to be an inflammatory disorder related to 'over-activation' of the immune system.
Psoriasis most commonly presents as symmetrical red, scaly patches and plaques on the elbows, knees, lower back and scalp, although any part of the skin can be involved including the palms and soles, skin creases and genital area. It can also affect the nails, and occasionally the joints (psoriatic arthritis).
There are several different types of psoriasis, which vary in their appearance. These include:
Psoriasis is a chronic inflammatory skin condition characterized by well-defined, red patches or plaques (thickened skin) often with a silvery scale, which may or may not be itchy.
Psoriasis can start at any age including childhood, but is most common in adulthood. It affects males and females equally and about one third of patients have a family history of the condition. Although genetic factors are important, the disease is thought to be an inflammatory disorder related to 'over-activation' of the immune system.
Psoriasis most commonly presents as symmetrical red, scaly patches and plaques on the elbows, knees, lower back and scalp, although any part of the skin can be involved including the palms and soles, skin creases and genital area. It can also affect the nails, and occasionally the joints (psoriatic arthritis).
There are several different types of psoriasis, which vary in their appearance. These include:

 Children require special care in many areas, and their skin health is no exception. Children are more prone to certain dermatological conditions, which can be distressing if not managed properly. These include eczema (dermatitis), infections such as impetigo, viral rashes, warts and psoriasis. Dr Andrew Ming specializes in the treatment of all aspects of Paediatric Dermatology and offers a comprehensive range of services specifically for children and adolescents.
Children require special care in many areas, and their skin health is no exception. Children are more prone to certain dermatological conditions, which can be distressing if not managed properly. These include eczema (dermatitis), infections such as impetigo, viral rashes, warts and psoriasis. Dr Andrew Ming specializes in the treatment of all aspects of Paediatric Dermatology and offers a comprehensive range of services specifically for children and adolescents.